Before we begin, some important mentions:
- This English version of the article is a translation of the original version in Romanian, published by the same author on the DoctorMiT medical portal.
- To jump between sections, use the Table of Contents. You can bring it back into view at any time by clicking on the icon stating Article Index appearing on the right of the screen.
- The author of this article is NOT a medical professional and the contents of this article is written for EDUCATIONAL PURPOSES ONLY. However, the article has been reviewed by several medical professionals and no concerns were flagged about any inaccuracy or presence of information contradicting medical facts.
What exactly is ADHD?
First of all, you’re probably wondering: what exactly is ADHD? The acronym stands for “Attention Deficit / Hyperactivity Disorder”.
In the US, the terminology ADD (an acronym for Attention-Deficit Disorder) is also used. This refers to the subtype of the condition in which hyperactivity is not present (the inattentive type), but in most countries both forms fall (slightly confusingly) under the same umbrella of ADHD.
ADHD is a neurodevelopmental disorder. People with ADHD show symptoms of difficulty maintaining attention, hyperactivity and impulsivity. ADHD occurs due to damage to the child’s brain during intrauterine fetal development, at birth or after birth. It is a commonly mentioned but incompletely defined and often inaccurate condition, which has maintained a general confusion about exactly how it manifests and what causes it.
For example, it is believed that the condition is simply an individual’s inability to pay attention. Although this is one component of the clinical picture, many more defining aspects of this condition affect patients in all areas of their lives involving executive brain functioning. Although ADHD in children is more commonly diagnosed than ADHD in adults, it can affect anyone, regardless of gender, sexual orientation, age, or any other characteristic.
People with this condition are at increased risk of self-isolation and developing a persistent sense of self-hatred if they believe that they are consciously responsible for their reduced ability to concentrate and that everything could be fixed if they just “tried hard enough”.
What is interesting is that ADHD itself is not necessarily their biggest problem, as it is treatable. Dr Russel A Barkley, the author of the book “Taking Control of Adult ADHD” and an international authority on ADHD, said in a public seminar:
The beauty of ADHD is that it is the most treatable condition in psychiatry. There is no other condition that offers so many possibilities for drug treatment and psychosocial interventions, and that has such a significant positive impact. Did you know that the medications used in standard treatment for ADHD produce 4 times more change than the antidepressants and anxiolytics you offer like candy in your practice?
Dr Russel A Barkley, the author of the book “Taking Control of Adult ADHD”
You can watch the fragment of Dr Barkley declaring that at minute 14:45 in the video about ADHD created by the author of this article:
Complications arise when people are misdiagnosed or when their diagnosis is misunderstood socially. A general negative view of the syndrome can lead to painful internal struggles (cognitive dissonance). This is especially true when a person who experiences symptoms of ADHD daily, which they can hardly control, hears at least one of the following statements from those around them:
- their manifestations are the result of his choices, and they just need to try harder
- their behaviour is labelled as destructive or inappropriate
- their behaviour is the result of a poor upbringing
Over time, unresolved inner conflicts encountered in affected individuals can generate persistent feelings of inadequacy. Without appropriate treatment, the person with undiagnosed ADHD remains trapped in a vicious circle of helplessness, where self-loathing becomes a constant.
While conservative studies place estimates of the percentage of adults affected by ADHD at 6-7% (Valsecchi P. et al., 2021), other estimates exceed the 10% threshold or even 16% (La-Malfa et al., 2008). While these statistics do not seem unheard of, many of the fairy tales and stories that have spread over the years continue to circulate today, perpetuating the stigma of the diagnosis and medication associated with ADHD. The effects of stigma often take the form of chronic anxiety, depression, or even suicidal thoughts.
Worst of all, these myths discourage people from taking their condition seriously, seeking the services of an expert for a thorough assessment, or accessing treatment that would improve their quality of life. One thing to bear in mind is that all these fears that people have and the fear of taking action to get a diagnosis and treatment are different from the results of an unfavourable context or lack of scientific evidence. On the contrary: The American Medical Association noted:
ADHD is one of the most well-researched disorders in medicine, and the overall data on its validity is far more convincing than that for most mental disorders and even for many medical conditions.
Reference: Polanczyk, G. V. et al, 2012
To contribute to solving this problem, we have listed and elaborated on some of the most common ADHD myths below in the hope that readers of this article will pass the information on.
Myth 1: “ADHD doesn’t exist. It’s a made-up condition! ADHD symptoms are seen in everyone!”
The most common myth about ADHD is that ADHD is a made-up condition. At a popular level, the reasoning starts from the observation that a multitude of people around us show symptoms of lack of concentration caused by excessive environmental distractions.
It is popularly believed that the cause lies within the context of the modern hyper-connected world, which bombards us with notifications, flashing ads and messages from multiple directions. To understand that these distractions have nothing specifically to do with the modern world, we need to look at the history…
A brief history of ADHD
Early mentions of what the DSM-IV defined as “ADHD” were described as early as the 17th century. Back then, there was no question of modern world distractions like notifications, social media, or bright advertisements.
1775 – Dr. Melchior Adam Weikard vaguely describes “inattention”
In 1775, Melchior Adam Weikard published in German the work “Attention Deficit” (Mangel der Aufmerksamkeit, Attentio Volubilis) (Barkley, A. & Peters H., 2012).
In his book, Weikard describes several symptoms of inattention, giving more details that closely match the disorder we know today. At the same time, many of Weikard’s observations stand up to modern scrutiny, as reviewed by Barkley, A. & Peters H., 2012 and Martinez-Badía J, 2015.
Weikard characterises a person with “inattention” as a person distracted by everything, even their imagination, putting more effort into tasks, fickle, sloppy, having the resulting work with many errors and generally disorganised.
He also refers to what today we call impulsiveness in a manner which fits the DSM-V diagnostic criteria for inattention and suggests criteria for hyperactivity and impulsivity.
1798 – Dr. Alexander Crichton formally defined attention
In 1798, Dr Alexander Chricton of Edinburgh, Scotland, published his paper entitled “An Inquiry into the Nature and Origin of Mental Disorders”. He gave the first formal definition of attention, laying the foundation for the diagnosis of ADHD:
When any object of external sense or of thought occupies the mind to such a degree that a person receives no clear perception from any other one.
Dr. Alexander Crichton, 1798
Elaborating, Crichton said:
If it can, with propriety be called so, every impression seems to agitate the person and gives him or her an unnatural degree of mental restlessness: people walking up and down the room, a slight noise in the room, the movement of a table, a sudden closing of the door, a slight excess of heat or cold, too much light or too little light, all destroy constant attention in such patients.
Dr. Alexander Crichton, 1798
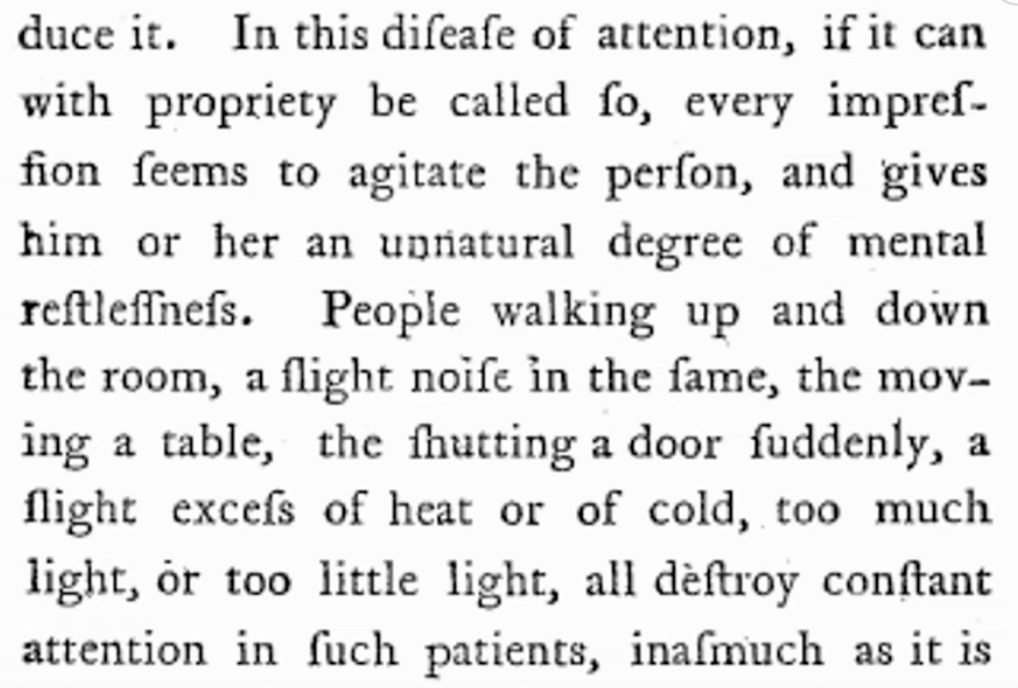
Linguists believe that the historical period corresponding to Crichton’s patients is where the term fidgets comes from:
It gives them vertigo and headaches and often causes such a degree of anger that borders on insanity. When people are affected in this manner, which they very frequently are, they have a special term for the state of their nerve, which is expressive enough of their feelings: they say that they have the fidgets.
Dr. Alexander Crichton, 1798
We travelled back in time to interview Alexander Crichton. You can watch the interview starting at minute 4:26 of the introduction video created by the author of this article:
1845 – Dr. Heinrich Hoffmann introduced the term “Attention Deficit Disorder” (ADD)
In 1845, the German physician Heinrich Hoffmann published a book called “Der Struwwelpeter” (The Story of the Fickle Philip), which featured a boy who could not sit still. This book helped raise awareness of ADHD and introduced the term “Attention Deficit Disorder” (ADD).
Where do we stand after some 350 years?
More than three and a half centuries after it was first mentioned in the scientific literature, there is, unfortunately, much doubt, both among the members of the public and medical professionals, that ADHD is an actual medical condition.
The book ADHD Does Not Exist, written by Richard Saul M.D., argues that ADHD is an incorrectly defined syndrome that should not be treated as a disease but rather a complex set of symptoms caused by over twenty different conditions, each of which requires different treatment. The author does not seem to offer any solid counter-arguments but makes a claim worthy of questioning his academic, professional, and, not least, personal integrity:
ADHD is an excellent excuse. Diagnosis can be an easy crutch to reach. Moreover, there is an element of attraction to an ADHD diagnosis, especially in adults. It can be exciting to think of yourself as being involved in many things simultaneously, rather than being stuck in a boring routine.
Author of the book ADHD does not exist
We see no point in elaborating further, as this statement, regardless of context, denotes an “a priori” denial of the concept of impairment of executive functions responsible for focusing on a single task at a given time.
How well-studied is ADHD?
Since the 16th century, over 120,000 clinical publications have been published on this topic (Barkley, 2015), reporting significant differences between individuals where ADHD is present and those where it is not (Roberts et al., 2015).
The accuracy of the information on the number of scientific articles available can be checked by performing a specific search on a specialised search engine such as sCite or Google Scholar by performing a search such as:
(adhd) OR (attention deficit hyperactivity disorder)

Numerous studies have found that ADHD is associated with structural and functional changes in the brain, such as reduced activity in the prefrontal cortex, an area of the brain involved in most executive functions affected by ADHD.
Curatolo, P., D’Agati, E., & Moavero, R., 2010, in their paper entitled “The neurobiology of ADHD”, list the main areas of functionality affected by ADHD:
- problem solving
- planning and orienting
- vigilance
- cognitive flexibility
- sustained attention
- response inhibition
- working memory
- motivation
- delay aversion
You can view a short interview with Dr. Paulo Curatolo, lead author of this manuscript, starting at minute 8:06 of the ADHD introduction video made by the author of this article:
According to another study, MRI scans of people with ADHD show that the cortex, or outer layer, is thinner in frontal regions and reduced in volume in the inferior frontal gyrus and the occipital and temporal lobes (Matthews et al., 2014).
Another form of this myth: “So-called ADHD symptoms are just an excuse for laziness/lack of willpower. You just have to try harder!”
If you have ever heard these sayings, you are probably not alone. People with mental health problems, especially those who have ADHD, are often called lazy by others, and this can have negative implications. They may feel rushed or find they lack the energy to cope with stressful situations. Others may perceive them as lazy, even though they do not have the energy to complete tasks.
While it may be easy to understand how someone lacking motivation could be perceived as lazy, it is essential to remember that this is not the reality.
Are people with ADHD really lazy?
As the manuscripts mentioned above report, executive functions are impaired at the neurological level, making it impossible for a person with ADHD to perform tasks more efficiently than the level of dopamine and noradrenaline in the prefrontal cortex, i.e. the inter-synaptic/inter-neuronal space, allows.
In a social media post, one patient states:
Telling people with ADHD to “get up and do your job!” is like telling a paraplegic to walk without a wheelchair. I could describe medication as “my wheelchair”.
Reddit anonymous user
We believe that the empirical evidence referenced should be sufficient to cover this myth. So, we conclude this point by summarising: contrary to widely held stories, ADHD is not simply laziness and the need to try harder but is a neurological disorder that can have a significant and chronic impact on a person’s life in all aspects of executive functioning, vital in both the professional and personal settings.
Myth 2: “Adjustments and means of treatment for ADHD for those with a diagnosis are an unfair advantage”
It is often perceived that adjustments offered to ADHD patients may give them an unfair advantage over others. For example, one might consider that the extra time provided to complete a task may give an advantage over a person who does not have ADHD and does not have the same privilege.
However, this is a logical fallacy since, as the manuscripts cited above mention, for people with ADHD performing specific tasks involve more effort, and they perform tasks more slowly to avoid mistakes.
The extra time given to a person with ADHD is intended to allow them to perform a range of tasks to the same standards as a person without ADHD, who does not have to make an extra effort to concentrate while simultaneously trying to ignore intrusive thoughts or noises in the environment.
Does ADHD medication make you superhuman?
Also, this unfairness bias stems from information that drugs used to treat ADHD improve cognitive abilities, but this does not apply in all cases, as the effects of ADHD medication can vary from person to person. Some people may find that medication helps them think more clearly and be more productive. In contrast, other patients may not notice any significant difference.
Medication alone is unlikely to give anyone an unfair advantage over others. Also, while a person without ADHD might feel euphoric or hyper-energetic under the influence of stimulant medication, in most cases, medications only make neurodivergent people function sustainably to achieve their daily goals.
Therefore, the adjustments offered to people do not seem to give them an unfair advantage but rather just specific adaptations or modifications. They only balance the conditions of the ‘social game’ so that everyone has an equal chance of success.
Myth 3: “ADHD in adults? Only ADHD in children I’ve heard of!”
A recent meta-analysis of the scientific literature on estimates of the proportion of ADHD cases in adults concluded that, at least symptomatically, the percentage of those affected is between 2.52 and 8% (Song et al., 2018).
While ADHD is a condition commonly diagnosed in childhood, it can also affect the lives of adults, especially if they have not been diagnosed before the age of majority.
The statistics on the diagnosis rate among children, which significantly exceeds that of adults, could also have as a subsidiary cause the policies on diagnosis and treatment of ADHD. Typically, these give higher priority to children with ADHD, with an emphasis on early diagnosis.
The statistics on the diagnosis rate among children, which significantly exceeds that of adults, could also be a subsidiary cause of the policies on diagnosing and treating ADHD. Typically, these give higher priority to children with ADHD, emphasising early diagnosis.

Another form of this myth: “ADHD and attention deficit symptoms are overcome once you get past the toddler stage!”
Much debate is centred around this controversial topic: whether ADHD may eventually disappear because it can be overcome. Research suggests that in most cases, untreated ADHD in childhood continues to make its presence felt in adulthood and may even continue to do so throughout life.
Some adults show symptoms very similar to those of children: fidgeting, squirming or having difficulty sitting still. Problems managing and expressing emotions noticeable lack of concentration are typical of ADHD symptoms commonly seen in adults.
Are there any other causes or types of ADHD other than that experienced from birth or early childhood?
Some research indicates that there are cases in which adults working in certain occupations where their brains endure sustained oxygen deprivation show symptoms similar to those experienced by a person with ADHD. Researchers also point to cases where ADHD-like symptoms occur in adults working in certain occupations where their brains endure sustained oxygen deprivation.
A study of girls aged 6 to 12 diagnosed with ADHD as children found that ten years later, they continued to have higher rates of ADHD and co-existing conditions than girls without ADHD, including higher rates of suicide attempts and self-harm (Hinshaw et al., 2012).
Another longitudinal study of children with ADHD indicated that, of the cases analyzed, 50-80% had ADHD during adolescence, and 35-65% continued to meet diagnostic criteria even as adults (Owens et al., 2015). Likewise, another study conducted on boys diagnosed with ADHD during childhood found that 77% still met DSM-IV clinical criteria for ADHD at the time (Biederman et al., 2012).
Although more research is needed to understand the condition entirely, it can significantly impact an individual’s life, and its magnitude should not be dismissed as just a stage of childhood.
Myth 4: “The child with ADHD can only be a boy!”
Indeed, it is estimated that ADHD is diagnosed twice as often in boys and males as in girls and females. It is believed that this occurs because boys and males with ADHD are more likely to show symptoms of hyperactivity and impulsivity. However, this does not mean that girls cannot have ADHD but are less likely to be diagnosed. This discrepancy may be caused by the fact that symptoms are more easily overlooked among females, as they mask their symptoms because of social expectations about their behaviour.
Some studies show atypical results, finding that girls are three times more likely to be diagnosed with ADHD than boys, and girls with ADHD are more likely to fall into the inattentive ADHD subtype. ADHD subtypes are discussed in detail in section Myth 6.
Hinshaw et al., 2012 conducted a follow-up survey of young girls aged 6 to 12 to find that they were at higher risk of suicide attempts and self-harm than boys. Other studies have shown that there is a 2.5:1 gender difference at these ages but that when they reach adulthood, the prevalence of the disorders is similar for both sexes (Owens et al., 2015).
Myth 5: “ADHD is a life sentence”

While many children with ADHD can lead everyday lives, others are more affected. Parents and carers should offer support and guidance, remembering that those with ADHD are more likely to struggle to reach their full potential.
Available treatment methods are abundant. Alongside medication for ADHD, psychotherapeutic intervention through therapies, such as Transactional Analysis (TA) and Cognitive Behavioural Therapy (CBT), prove to be particularly effective as part of a holistic ADHD treatment plan, especially when undertaken alongside medication.

Myth 6: “ADHD necessarily means hyperactivity. If you’re not hyperactive, you can’t possibly have ADHD.”
Perhaps the acronym for the condition should be expanded from “attention deficit hyperactivity disorder” to “attention deficit or hyperactivity disorder” or even replaced with “executive functioning deficit disorder” as it would more accurately reflect the broad field of manifestations and subtypes of the condition.
There is more than one type of ADHD:
- ADHD type in which hyperactivity predominates (this type of ADHD includes specific symptoms of agitation, restlessness and motivational problems – 35% of cases)
- predominantly inattentive ADHD type (15% of cases)
- combined ADHD (the remaining ~50% of cases).
The inattentive type includes symptoms such as poor concentration, distractibility and forgetfulness. This type of ADHD in boys/men is more common than in girls/women. Symptoms of ADHD include avoidance of activities that require deep thought, inability to maintain concentration for long periods, forgetfulness, inattention and low energy.
These people are usually creative and intelligent, but ADHD often hurts their academic or professional performance. This category of ADHD is often overlooked, but it can be treated as effectively as the others and may respond even better to stimulant medication.
Myth 7: “Those people with ADHD can’t concentrate on anything!”
Maintaining focus on a tedious task can be difficult for people with ADHD. This disorder affects the executive functions of the brain, which work best when a task or activity is new and exciting. So people with ADHD have significant problems staying focused on tedious tasks and have to learn to moderate it.
When faced with a tedious task in the school environment, a child with ADHD tends to jump from one task to another or skip essential steps in a procedure. They also need help to organise their homework and maintain attention in a noisy environment.
In the work environment, adults with ADHD are also at risk of boredom. Many jobs involve long periods of sitting down and looking at documents. They can also get bored in group sessions, primarily when they deal with abstract topics. Boredom can also lead to inappropriate behaviour in a professional context, such as shouting, humming, and joining in irrelevant conversations.
However, people with ADHD are usually able to focus on activities that are highly engaging or stimulating, having what is called “hyper-focus” because ADHD neurologically translates into the inability of the executive function to perform its role: setting and resetting priorities in real-time.
Myth 8: “People with ADHD cannot be highly intelligent”
There is no clear consensus that ADHD is a learning disability. Some experts believe that ADHD may be a co-existing condition with learning disabilities. Others believe the two are separate conditions.
However, it is agreed that ADHD can hinder learning and affect individuals’ academic or professional success. Many people with ADHD have difficulty with executive functioning skills, such as organisation and time management, which can make it challenging to keep up with schoolwork. In addition, they may also have impulsivity and distraction problems, which makes it difficult to pay attention in class, memorise knowledge quickly and assimilate new information. Although affected individuals generally have difficulty in school because of the symptoms mentioned above, there is no evidence that people with ADHD are less intelligent.
The 8 types of human intelligence

It should also be remembered that intelligence is of more types than the one popularly equated with understanding, namely cognitive intelligence. According to the theory of multiple intelligence developed by Dr Howard Gardner, there are eight distinct types of intelligence:
- verbal intelligence
- logical-mathematical intelligence
- spatial intelligence
- musical intelligence
- kinaesthetic intelligence
- interpersonal intelligence
- intrapersonal intelligence
- natural/environmental intelligence
Intelligence is, therefore, much more diverse than an IQ test can measure.
World leading personalities with ADHD
While people with ADHD often struggle with the underlying elements of their condition, they can be brilliant in other areas. For this reason, many specialists recommend strengths-oriented therapeutic approaches that focus on awareness and development rather than on fighting ADHD-specific behaviours.
Further confirmation can be given by the 91 personalities collected on the Getinflow website, including astronaut Scott Kelly and writer Mel Robbins. Watch a video of Scott Kelly at minute 15:47 of the video entitled The beauty of ADHD:
At the same time, according to extensive behavioural analyses based on written historical sources and medical records, specialists and researchers believe that personalities such as Wolfgang Amadeus Mozart had typical ADHD manifestations (Schmitt et al., 2014).
A recent study published in Psychological Medicine looked at academic outcomes among people with ADHD. The study also looked at subjects’ IQ scores and determined that, indeed, patients with ADHD tend to score higher on IQ tests. According to the results, they are likelier to notice similarities and differences between concepts. They also make correlations between multiple ideas and concepts in a relatively short time, a trait of people with strong intellectual capacity.
Myth 9: “ADHD is the cause of poor education”
The precise set of causes for ADHD is unknown, but what is known is that poor home education is not necessarily the cause. Various experts believe that genetic and environmental factors are involved in ADHD. Although poor parenting may contribute to some symptoms of ADHD, it is not considered the root cause of the disorder.
Indeed, ADHD runs in families, but the causes are thought to be genetic rather than educational. If one parent has ADHD, there is a 57% chance that their child will suffer from it. In the case of twins, if one twin has ADHD, the other has a 70%-80% chance of having it, too (Barkley, 2015).
Researchers have identified genetic and neurological factors as the leading causes of ADHD, with social factors such as poor parenting playing a minimal role. Studying twins with ADHD, researchers have found that individual differences in symptoms can be attributed to genetic factors, with siblings of children with ADHD having a 30% chance of also having the disorder and family environment having a negligible impact (Barkley, 2015).
Myth 10: “Sugar consumption can cause or worsen ADHD”
Parents tend to believe that sugar can cause hyperactivity in children with attention deficit hyperactivity disorder. However, according to the latest research, this claim lacks solid scientific support. In some cases, parents or others may notice hyperactivity in their child after eating foods high in sugar. However, it is essential to note that this is only a correlation, not a cause-and-effect relationship.
What do studies say about sugar and ADHD?
Some experts believe that a sugary diet contributes to hyperactivity and impulsivity, suggesting a link between sugar and ADHD because it can cause blood sugar spikes, leading to mood swings and difficulty concentrating.
A recent study showed that high sugar consumption is associated with a higher risk of ADHD in boys. However, another study showed that the persistence of high sugar consumption between the ages of 6 and 11 was not associated with a higher risk of ADHD but instead suggests a reverse causality: increased sugar consumption among children with ADHD may result from the disorder itself.
Dr Barkley mentioned in a public seminar that glucose in the liquid form helps people with ADHD during a task involving prolonged executive effort, such as an exam, as they naturally have a glucose deficit in the frontal lobe.
What diets are recommended?
Eating foods high in protein is also beneficial for those with ADHD. Protein helps the body produce neurotransmitters, which help brain cells communicate.
A 2014 study determined that an elimination diet might show promising results in some children, such as those with allergies. Another 2016 review conclusively determined that a gluten-free diet is not recommended as a standard treatment for ADHD.
For parents who suspect that their child’s diet may contribute to ADHD symptoms, the American Academy of Pediatrics recommends limiting sugar intake to less than 10% of daily calories or six teaspoons per day for children aged two to 19. This restriction is based on a sample of 28 children.
Myth 11: “ADHD is overdiagnosed!”
There is a standard view that ADHD is overdiagnosed. This misconception can make it seem that if a person is undiagnosed, they are not struggling with ADHD. However, the reality is that many adults who have ADHD struggle to access proper care because of the stigma. The more we know about ADHD, the easier it will be for people experiencing symptoms to seek help and find the support they need.
According to Dr Michael Mier, a psychologist and lecturer at Webster University, “ADHD is the most commonly diagnosed behavioural disorder among children.”. Dr Mier described general public awareness of ADHD as “very low,” confirming that many people do not know about ADHD and how it can affect their lives.
Dr Khaled Helmy, a consultant psychiatrist at Ciconia Recovery in London, said, “Treating ADHD is difficult mainly just because it is difficult to diagnose, largely due to lack of awareness, which makes people sceptical.” He also said that 75% of adults remain undiagnosed and reach the end of their lives, not knowing why they have had problems at school, at work, or with their partner.
Dr Barkley also affirms in the same video where he mentions that ADHD is the most treatable condition, that 40% of children and 90% of adults do NOT get treatment. You can watch the portion of the video again here.
How accurate is the diagnosis of ADHD?
Only a qualified specialist psychiatrist can formally and objectively diagnose ADHD. Pre-diagnostic assessment includes an extensive set of questionnaires and interviews for anamnestic purposes and numerous cognitive assessments covering the full range of executive and cognitive functions. Therefore, the chances of people being diagnosed with ADHD when they do not, in fact, have the condition are pretty slim, or at least certainly slimmer than for other conditions. In the rare cases where this does happen, there are various causes, such as:
- some people look for a quick solution or explanation for their problems.
- inadequate or incomplete assessment methods are adopted by certain specialists.
- the training of medical and mental health professionals in assessment methodology and differential diagnosis is inadequate or incomplete.
What causes the rapid rise in the number of diagnosed ADHD cases?
The percentage of children identified with ADHD has increased by about 5% each year, according to the National Survey of Children’s Health, conducted annually from 2003-2011. Because of this accelerated increase, many have wondered whether the condition is overdiagnosed.
We do not think this concern is well-founded, as the report based on the 2014 National Study on the Diagnosis and Treatment of ADHD and Tourette Syndrome found that health professionals diagnose children very carefully. According to Visser et al., 2015, of the 2976 children who received these diagnoses, 9 out of 10 were given by practitioners using best practice guidelines.
Several reasons contribute to the rise in ADHD diagnoses, such as:
- health professionals and parents are more aware of the condition
- more examinations are performed by paediatricians and other primary care nurses
- there is a decrease in the stigma surrounding ADHD
- there have been significant recent improvements in treatment options
- there has been an increase in referrals triggered by environmental factors such as prenatal exposure to toxins or elevated blood lead levels.
So we can see that the reasons for the increase in the number of cases diagnosed with ADHD are legitimate and should not arouse suspicion.
Myth 12: “There’s no point in being diagnosed as an adult. To treat ADHD you have to be diagnosed as a child”
People with ADHD often feel ashamed of their condition and believe they are worthless. This belief is particularly devastating for adults, who may feel their condition makes them no better or more appropriate than their friends, partners or co-workers. They may also see themselves as subject to a hoax of fate, which is particularly damaging.
Instead of viewing their condition as a travesty of fate, we believe it would help them to see it instead as a legitimate need for help and treatment. Many adults struggle without a diagnosis, and this can hold them back. However, unfortunately, there is still debate among professionals about whether it makes sense to be diagnosed as an adult anymore.
How does an ADHD diagnosis help you as an adult?
We believe it is significantly beneficial for an adult to be diagnosed as an adult! Receiving a diagnosis regardless of age can help people better understand themselves and their unique brains. It can also alert loved ones and their doctor to problems that may arise or even uncover other adjacent health conditions.
In addition, many adults with ADHD find that getting a diagnosis helps them feel like they “fit in” somewhere because they are no longer alone in their struggles and finally get the diagnosis and support they need. The latter is, in most countries, specified even within legal provisions but is not precisely guaranteed in the absence of a formal diagnosis.
Ultimately, whether or not one wishes to diagnose and treat ADHD as an adult should be a personal decision. What is certain is that discouraging people from participating in the ADHD evaluation process is not beneficial to anyone. Instead, it is a harmful approach that only perpetuates the lack of awareness of this condition.
Myth 13: “Vitamins and other nutritional supplements can treat ADHD”
Vitamins are proven ineffective in treating the disorder and may exacerbate some of its symptoms if taken with other medications that treat ADHD.
For example, stimulant drugs improve alertness, making them practical for children and adults who need help concentrating and paying attention.
Vitamins such as methylcobalamin (vitamin B12) or folic acid, taken on their own, do not have this effect because they do not affect dopamine or serotonin levels in the brain enough to be considered therapeutic. They do not trigger improvements in behaviour that can be said to be clinically significant.
Myth 14: “ADHD medication is dangerous!”
It is true that, as with any drug, there is always the potential for abuse and addiction. However, the risks of stimulants prescribed for ADHD being addictive are small compared to other drugs. This feature particularly applies to the latest generation: extended-release formulations such as Lisdexamfetamine (Elvanse / Vyvanse) or extended-release Methylphenidate (Concerta). They pose a much lower risk of abuse than the instant-release versions.
According to the SAGE Encyclopedia, amphetamine was discovered in 1887 by the Romanian chemist Lazăr Edeleanu. It was approved for medical use in 1933. It was administered as an inhaler to dilate the bronchial tubes in lung diseases. With the advent of dextroamphetamine sulphate, the substance started to be used to treat various psychiatric conditions. Lisdexamfetamine, used today to treat ADHD, is composed of the amino acid L-Lysine and Dextroamphetamine, the right-handed enantiomer of Edeleanu’s racemic amphetamine formula.
In fact, extended-release dopaminergic medication could be the only way out of addiction for many patients. This potential applies even when talking about high-risk drugs such as cocaine. Both methylphenidate (Moeller et al., 2014) and lisdexamfetamine (Mariani J et al., 2021) exhibited great potential in this area.
Stimulants are generally considered safe and effective courses of treatment for ADHD and have been used for decades. According to a study by Lakhan, S. E., & Kirchgessner, A., 2012, medication treatment for ADHD has a success rate of over 80%.
Dr Barkley said in a public seminar:
In the past, protocols used to specify that we should try everything on the face of the earth and only then move on to medication as a last resort. Guess what? 80% of the time, we failed. That is why the protocols were changed, and now medication is the first line of treatment. Individuals are not susceptible to psychosocial interventions unless without medication, which applies both to adult ADHD and child ADHD.
Dr Russel A Barkley, CADDRA conference
In humans with ADHD, pharmaceutical amphetamines at therapeutic dosages appear to improve brain development and nerve growth. Reviews of magnetic resonance imaging (MRI) studies suggest that long-term treatment with amphetamine decreases abnormalities in brain structure and function found in subjects with ADHD and improves function in several parts of the brain, such as the right caudate nucleus of the basal ganglia. (Hart et al., 2013; Spencer et al., 2013; Frodl et al, 2012).
Basal ganglia regions like the right globus pallidus, the right putamen, and the nucleus caudatus are structurally affected in children with ADHD. These changes and alterations in limbic regions like ACC and amygdala are more pronounced in non-treated populations and seem to diminish over time from child to adulthood. Treatment seems to have positive effects on brain structure.
Frodl et al, 2012
Are ADHD medications dangerous for the heart?
Constantin-Cristian Topriceanu, a researcher at the Institute of Cardiovascular Diseases at University College London and a graduate of Cardiff University Medical School, together with three other researchers, conducted a thorough review of the scientific literature on the cardiovascular risks to users of both stimulant and non-stimulant ADHD medication (Topriceanu et al., 2022).
In an interview with AboutADHD, he said:
Although stimulants can promote an irregular heart rhythm, also known as arrhythmia, there is no convincing evidence linking ADHD drugs to heart attacks, strokes and cardiac arrest in the general population. In addition, most cardiovascular conditions, such as most valve problems and congenital heart disorders, are not contraindications for ADHD treatment.
However, there are certain conditions (e.g. those at risk of arrhythmias) where the use of pacemakers remains controversial, and there is insufficient data to encourage or discourage their use. However, for most patients, non-stimulants such as atomoxetine, guanfacine or clonidine are a perfectly valid option, as they have not been associated with arrhythmias or dangerous increases in heart rate.
Although ADHD medication significantly improves social, academic and occupational performance, many individuals with ADHD continue to be deprived of ADHD medication due to overly cautious approaches unsupported by evidence. However, our review shows that stimulant and non-stimulant medications for ADHD generally have good cardiovascular safety profiles. Nevertheless, given their mechanisms of action, they should be used with caution in children and adults with proarrhythmic heart or heart failure.
Conclusions
We will try to summarise the key points that we think readers of this article should be left with:
- ADHD can affect all people, regardless of gender, sexual orientation, age, or any other characteristic.
- ADHD is a treatable condition. It is even considered the most treatable of all neuro-psychiatric conditions.
- Society globally faces a serious lack of awareness about ADHD. People with symptoms need to understand the importance of a timely specialist assessment.
- Society globally faces a severe lack of awareness about ADHD. People with symptoms need to understand the importance of a timely specialist assessment.
- Most children with ADHD have a variety of difficulties, both at school and home.
- Many adults with ADHD also have problems with families, partners, or employers. 75% of them remain undiagnosed throughout their lives.
- Early diagnosis expands the range of treatment options available and prevents the condition from worsening and developing complications over time.
- According to longitudinal research, available drug treatment shows a safe and sustainable long-term pharmacological profile. This applies if it is administered according to treatment schedules established by a specialist.
What to do?
For the broader good of society, we should do all we can to raise awareness of ADHD. It is important to remember that we are dealing with an actual condition. It can make it challenging to carry out everyday life, not just complex tasks. We urge the readers to get the following message out to as many medical professionals and members of the public as possible:
ADHD is real, can affect anyone, regardless of gender, age, or any other characteristic, and is one of the most studied and treatable psychiatric conditions.
Andrei Hodorog, the author of this article
You can share this article! Chances are at least one more person will find out, and then the news will spread virally. With enough viral vectors of scientific information, we can beat the myth viruses!
Bibliography
Barkley, R. A., & Peters, H. (2012). The Earliest Reference to ADHD in the Medical Literature? Melchior Adam Weikard’s Description in 1775 of “Attention Deficit” (Mangel der Aufmerksamkeit, Attentio Volubilis). Journal of Attention Disorders, 16(8), 623–630. https://doi.org/10.1177/1087054711432309
Barkley, Russell A. (2015). Etiologies of ADHD. In R. A. Barkley (Ed.), ADHD: A Handbook for Diagnosis and Treatment, 4th ed. (pp. 356–390). New York, NY: Guilford Press. https://psycnet.apa.org/record/2014-57877-001
Biederman, Joseph et al. (2012). Adult Outcome of ADHD: A Controlled 16-Year Follow-Up Study. Journal of Clinical Psychiatry 73(7):941–950. https://doi.org/10.4088/JCP.11m07529
Crichton, A. (1798). An inquiry into the nature and origin of mental derangement: on attention and its diseases. Journal of attention disorders, 12(3), 200-204.
Ellis, Brandi & Joel Nigg (February 2009). Parenting Practices and ADHD: New Findings Suggest Partial Specificity of Effects. Journal of the American Academy of Child & Adolescent Psychiatry 48(2):146–154. https://doi.org/10.1097/CHI.0b013e31819176d0
Ginsberg, Y., Hirvikoski, T. & Lindefors, N. Attention Deficit Hyperactivity Disorder (ADHD) among longer-term prison inmates is a prevalent, persistent and disabling disorder. BMC Psychiatry 10, 112 (2010). https://doi.org/10.1186/1471-244X-10-112
Frodl T, Skokauskas N (February 2012). “Meta-analysis of structural MRI studies in children and adults with attention deficit hyperactivity disorder indicates treatment effects”. Acta Psychiatrica Scandinavica. 125 (2): 114–126. doi:10.1111/j.1600-0447.2011.01786.x. PMID 22118249. S2CID 25954331.
Hart H, Radua J, Nakao T, Mataix-Cols D, Rubia K (February 2013). “Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication, and age effects”. JAMA Psychiatry. 70 (2): 185–198. doi:10.1001/jamapsychiatry.2013.277. PMID 23247506.
Hinshaw, Stephen P. et al. (2012). Prospective Follow-Up of Girls With ADHD Into Early Adulthood: Continuing Impairment Includes Elevated Risk for Suicide Attempts and Self-Injury. Journal of Consulting and Clinical Psychology 80(6):1041–1051.
La Malfa G, Lassi S, Berteli M, et al (2008) Detecting attention deficit hyperactivity disorder (ADHD) in adults with intellectual disability: the use of Conner’s Adult ADHD rating scales (CARS). Research in Developmental Disabilities, 29: 158-64. https://doi.org/10.1016/j.ridd.2007.02.002
Lakhan, S. E., & Kirchgessner, A. (2012). Prescription stimulants in individuals with and without attention deficit hyperactivity disorder: misuse, cognitive impact, and adverse effects. Brain and behavior, 2(5), 661–677. https://doi.org/10.1002/brb3.78
Mariani, J. J., Choi, C. J., Pavlicova, M., Mahony, A. L., Brooks, D. J., Grabowski, J., & Levin, F. R. (2021). Open‐label pilot study of lisdexamfetamine for cocaine use disorder. The American journal of drug and alcohol abuse, 47(3), 402-409. https://doi.org/10.1080/00952990.2021.1885677
Martinez-Badía J, Martinez-Raga J. Who says this is a modern disorder? The early history of attention deficit hyperactivity disorder. World J Psychiatry. 2015 Dec 22;5(4):379-86. https://doi.org/10.5498/wjp.v5.i4.379. PMID: 26740929; PMCID: PMC4694551.
Matthews, Marguerite et al. (2013). ADHD. Current Topics in Behavioural Neurosciences 16:235–266.
Merikangas, Kathleen et al. (2013). Medication Use in US Youth With Mental Disorders. JAMA Paediatrics 167(2):141–148, https://doi.org/10.1001/jamapediatrics.2013.431
Moeller, S. J., Honorio, J., Tomasi, D., Parvaz, M. A., Woicik, P. A., Volkow, N. D., & Goldstein, R. Z. (2014). Methylphenidate enhances executive function and optimizes prefrontal function in both health and cocaine addiction. Cerebral cortex, 24(3), 643-653. https://doi.org/10.1093/cercor/bhs345
Owens, Elizabeth et al. (2015). Developmental Progression and Gender Differences among Individuals with ADHD. In R. A. Barkley (Ed.), ADHD: A Handbook for Diagnosis and Treatment, 4th ed. (pp. 223–255). New York, NY: Guilford Press. https://psycnet.apa.org/record/2014-57877-009
Palmer, E. D., and Finger, S. 2001. An early description of ADHD (Inattention Subtype): Dr. Alexander Crichton and the „Mental Restlessness” (1798). Child Psychology and Psychiatry Reviews, 6, 66-73. https://doi.org/10.1111/1475-3588.00324
Pastor, Patricia N. et al. (2015). Association between diagnosed ADHD and selected characteristics among children aged 4–17 years: United States, 2011–2013. NCHS Data Brief, no 201. Hyattsville, MD: National Center for Health Statistics.
Polanczyk, G. V., Casella, E. B., Miguel, E. C., & Reed, U. C. (2012). Attention deficit disorder/hyperactivity: a scientific overview. Clinics, 67, 1125-1126. https://doi.org/10.6061/clinics/2012(10)01
Roberts, Walter et al. (2015). Primary Symptoms, Diagnostic Criteria, Subtyping, and Prevalence of ADHD. In R. A. Barkley (Ed.), ADHD: A Handbook for Diagnosis and Treatment, 4th ed. (pp. 51–80). New York, NY: Guilford Press. https://psycnet.apa.org/record/2014-57877-002
Russell, Abigail E. et al. (2015). Socioeconomic Associations with ADHD: Findings from a Mediation Analysis. PLoS One 10(6):e0128248. https://doi.org/10.1371/journal.pone.0128248
Schmitt, A., Falkai, P. Historical aspects of Mozart’s mental health and diagnostic insights of ADHD and personality disorders. Eur Arch Psychiatry Clin Neurosci 264, 363–365 (2014). https://doi.org/10.1007/s00406-014-0507-7
Spencer TJ, Brown A, Seidman LJ, Valera EM, Makris N, Lomedico A, Faraone SV, Biederman J (September 2013). “Effect of psychostimulants on brain structure and function in ADHD: a qualitative literature review of magnetic resonance imaging-based neuroimaging studies”. The Journal of Clinical Psychiatry. 74 (9): 902–917. doi:10.4088/JCP.12r08287. PMC 3801446. PMID 24107764.
Topriceanu, C. C., Moon, J. C., Captur, G., & Perera, B. (2022). The use of attention-deficit hyperactivity disorder medications in cardiac disease. Frontiers in Neuroscience, 16. https://doi.org/10.3389/fnins.2022.1020961
Valsecchi, P., Nibbio, G., Rosa, J., Tamussi, E., Turrina, C., Sacchetti, E., & Vita, A. (2021). Adult ADHD: Prevalence and Clinical Correlates in a Sample of Italian Psychiatric Outpatients. Journal of Attention Disorders, 25(4), 530–539. https://doi.org/10.1177/1087054718819824
Visser, Susanna N. et al. (September 3, 2015). Diagnostic experiences of children with ADHD. National Health Statistics Reports; no 81. Hyattsville, MD: National Centre for Health Statistics.